Originally published in FierceHealthcare
In my years practicing as a family doctor, one of my most visceral memories was the constant fretting over chronically ill patients who needed follow-up attention but had fallen through the cracks.
It wasn’t because of a lack of effort in trying to reach out to these patients. But my tracking system largely consisted of 4-by-6-inch index cards, each filled out with a patient’s name, health condition, follow-up need and filed by the due date in a recipe box on my desk. When we could carve out the time, a precious resource under the fee-for-service model, my staff and I would sift through the cards to review the plan of care and reach out to my patients.
This system didn’t exactly move the needle on population outcomes, but in practices across the country, clinicians have always striven to not lose track of patients who stray from the plan of care. True preventive care, particularly tertiary prevention, has been the healthcare industry’s trip to Mars—there is a desire to get there, but no one has quite figured out how, including how to pay for it.
The Affordable Care Act (ACA) was a landmark turning point. The sweeping legislation included provisions to ensure more individuals receive preventive services, improved access to care and created new models to coordinate care between multiple disciplines. It also included incentives that helped fund the adoption and implementation of technology needed to pivot to these new models. And while the ACA may once again be in political peril, the federal government seems intent, at least, on maintaining and expanding the value-based model the ACA introduced.
The most exciting example to me is the recent directive by the Department of Health and Human Services to “deliver value-based transformation to primary care.” This bold promise implies far more than just a new rule or guideline. In fact, the initiative—officially labeled CMS Primary Cares—will enable physician practices to finally invest in the systems and staff needed to deliver smarter care for their patients.
CMS Primary Cares, as it is currently proposed, will be made up of five different payment models, each designed to reimburse care for patients with chronic conditions. Depending on the model, providers will be paid upfront, every month, for each applicable patient. Another way of putting this: It funds the provider’s investment in retooling the practice to manage a population based on risk and urgent needs.
This is a crucial investment. After all, you can’t retool a factory without investing in new infrastructure, and the same applies here. The providers who will ultimately succeed in value-based care will be the ones who use upfront payments the way they are intended—to invest in making the shift to value-based care. The truth is, most of healthcare is good at helping people when they’re sick and in an emergency. The industry is not so good at keeping people well, which is value-based care’s foundational premise.
True practice transformation will require new payment models like those offered by CMS Primary Cares, new technology, new workflows, staff training and a lot of support. And then more support.
At Equality Health, the integrated delivery system where I work, we provide the tools needed by the practices that help them deliver proactive, value-based care. The providers in our network and clinics, for example, are specially trained to assess patients for behavioral, social and cultural risk factors that can derail even the best care coordination plan. Because we serve a large population of Latino patients, the curriculum focuses on incorporating values and cultural beliefs that have significant meaning to this population.
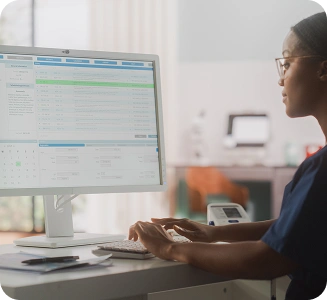
And in a thankful improvement from 4-by-6-inch cards, sticky notes and “pending” folders, we have our own proprietary care coordination platform that gives physicians real-time visibility into individual patient care gaps and population management performance. The platform pulls from many different data sources, including health information exchanges, so that the practice receives real-time admission/discharge/transfer alerts of patients to arrange prompt follow-up. It also gives a comprehensive view of the patient’s health and enables risk stratification, so that practices can easily review lists of patients, by condition or gap, who need to be scheduled for specific services.
The ability to track “at risk” patients and better coordinate their care is essential to improving outcomes. While it’s good to pay physicians differently, doctors can only be as effective as the information at their disposal. And this information can be very basic to begin with. Clinicians don’t need predictive analytics to query how many patients in their practice with uncontrolled diabetes are overdue for a blood pressure check and lab tests. They need to see the abnormal results and “outlier” cases, but they also need to know about the test that never got done. This is information that a care coordination system should display for the entire care team to see.
This kind of care can eventually extend to every patient—until, practice by practice, our healthcare system becomes one that is truly focused on proactive, preventive and coordinated care.
Payment reform has been a long time coming and will help physicians finally get off the hamster wheel of fee-for-service. With a new model that pays primary care providers to shift to value-based care, they can keep track of and provide the best possible care for every patient in their practice.