Independent primary care providers are drowning in a sea of documentation, insurance claims procedures, coding, billing and payer portals. Did you know that on average each practice has 12 payer portals to navigate? If you’re a primary care provider, we don’t need to tell you: Overwhelm and burnout rates are higher than ever. And, when administration takes up a disproportionately high portion of the workday, patient care and outcomes ultimately suffer.
Results from a 2022 Doximity poll indicate that 46% of physicians believe decreasing administrative burden would be the most effective intervention in reducing burnout. And, a study in the Annals of Internal Medicine found that physicians in outpatient settings spent almost half their workday (49%) on EHRs and “paperwork,” with many also working up to two hours every evening on administrative tasks. Neither practices nor providers can continue at this rate. Not only can we do better; it is imperative that we do better.
Value-based care is one area where administrative complexities can feel daunting. However, partners who offer effective solutions do exist and can be invaluable support to help bring meaningful value-based care tenets into the practice.
A care model such as Equality Health’s offers a version of value-based care that lightens administrative load and utilizes technology that simplifies administration rather than complicating it.
Wrangling payer portals just got easier
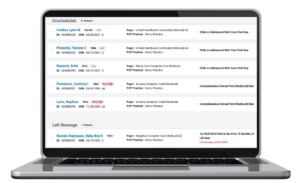
Equality Health’s technology platform presents actionable care opportunities and consolidates value-based care workflows, task lists, reporting and payments into a single, payer-agnostic environment. And, Equality Health gives practices this proprietary technology so they don’t have to invest in it themselves. CareEmpower® enables practices to monitor, track, and manage preventive care for their Equality Health attributed members all in one place. Practices track and monitor key preventive screenings, hospital alerts, and comprehensive data on high-risk patients in an easy-to-use format.
Get paid faster and more predictably
Unpredictable revenue streams are an additional source of stress and overwhelm for providers. Participating in Equality Health’s activity-based payment program enables providers to receive payments quarterly, eliminating the often long wait for value-based payments and paying providers up to five times faster than health plan reimbursement. Maximizing practice productivity, this activity-based payment program aligns with HEDIS and health plan quality goals.
Optimizing workflow
At times, it can be beneficial to have a set of outside eyes and ears. Our team works alongside practice staff to suggest ways to streamline workflows and adopt best practices for visits and chart prep. Our practice performance managers and tools can even help with prioritized worklists so practices can align to the clinical and quality measures that matter most to the practice. The goal? To help practices function more efficiently and more effectively, with improved patient outcomes.
Equality Health is on a mission to fix the problem
Equality Health is dedicated to provider success. As a key partner to both health plans and practices, Equality Health can assume downside risk and help improve both MLR and HEDIS scores. Participation in a model such as ours allows providers to regain control of their administrative responsibilities